Worldwide obesity rates have almost tripled since 1975. At the same time, rates of depression have steadily risen. Since the early 2000s, many studies have established a link between these two conditions, showing that the prevalence of depression in people with obesity is twice as high as in people of a healthy weight.
Part of the association is intuitive, says Elina Hyppönen, director of the Australian Centre for Precision Health at the University of South Australia in Adelaide. “Obese people experience stigma and that’s bound to affect mental health,” she says. The two conditions are also influenced by some of the same risk factors — including less-healthy eating habits, physical inactivity, disrupted sleeping patterns and substance abuse.
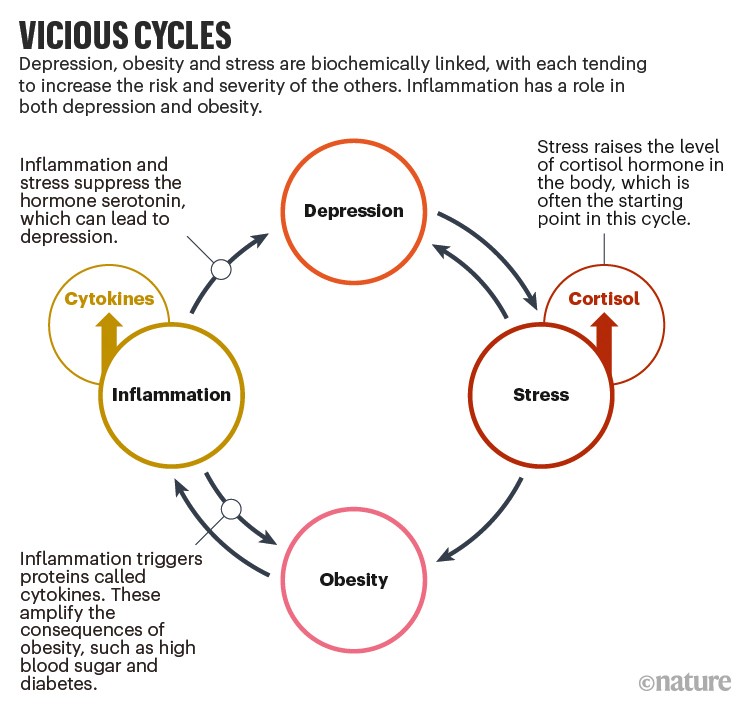
But in truth, the relationship between obesity and depression is much more complicated. Research over the past decade has described an intertwined and overlapping biochemical back-and-forth between the two conditions, with each conspiring to aggravate the other.
A double dose of inflammation
People with obesity often experience chronic inflammation. Fatty tissues house a range of immune cells, which produce signalling proteins associated with inflammation. People with obesity are therefore likely to produce an overabundance of these molecules. Some of these proteins, such as cytokines, are so closely related to mental-health problems that they’re commonly used as biomarkers for depression1.
Several studies have found that cytokines downregulate serotonin, a key hormone in mood regulation. They do this by stimulating an enzyme that alters the supply of amino acids needed to build serotonin.
The cytokine effect provides one biological explanation for why people with obesity are at greater risk of developing depression, but it cuts both ways (see ‘Vicious cycles’). Studies have also shown that people who are depressed, regardless of their physique, already have higher concentrations of cytokines in their bodies.
Pro-inflammatory cytokines can cause insulin resistance to develop, leading to type 2 diabetes. And, because people with this type of diabetes have an increased risk of gaining weight, it’s therefore equally possible that elevated cytokine levels caused by depression are contributing to obesity. “It’s a vicious circle,” says Hubertus Himmerich, a psychiatrist at King’s College London.
Stephanie Borgland, a neuroscientist at the University of Calgary in Canada, echoes that analysis. “Individuals with obesity and depression show increases in pro-inflammatory cytokines,” she says. “It’s almost impossible to say which is causing which.” In fact, she adds, both conditions are probably to blame for making the other worse.
The stress connection
Cortisol is often called the stress hormone because it’s produced under demanding or potentially harmful situations; cortisol increases blood sugar levels to supply the brain with more glucose. It’s a helpful response in the short term. But studies have shown that stressful biochemical conditions can be prolonged by the onset of mood disorders such as depression.
In 2016, for example, scientists observed the behaviour of 41 macaque monkeys (Macaca mulatta) for one hour per day over the course of 2 weeks. The researchers looked out for behaviour such as bowing the head or curling up into the fetal position, which were deemed to be potential indicators of depression. They also took hair samples, from which the scientists could gauge cortisol levels. Eighteen of the monkeys showed no signs of depressive behaviour and so were treated as the control group. The end results showed that the depressed group of 23 monkeys secreted significantly more cortisol than the control monkeys2.
Similar results have been seen in people. In a 2019 paper, researchers assessed the mental health of 89 men and took blood samples to measure cortisol. They found a positive correlation between cortisol levels and depression3.
This represents another key link between obesity and depression, says psychiatry researcher Valerie Taylor, who collaborates with Borgland at the University of Calgary, because cortisol has many roles beyond stress response — one of which is to increase appetite. “Cortisol production predisposes you to weight gain,” Taylor says. “There’s a self-soothing aspect to it. That’s why you crave chocolate ice cream when someone breaks up with you, and not carrots. Depression can mean a continuation of this.”
So, if depression increases cortisol, it stands to reason that obesity could be a knock-on effect. But, as with cytokines, the cortisol effect also flows in the other direction. Obesity, independent of depression, is also correlated with high cortisol concentrations. A meta-analysis that looked at obesity, but not depression, found that for every 2.5-point increase in body mass index, there’s a corresponding 9.8% increase in cortisol found in hair samples4. High cortisol — linked to depression — can fuel obesity. And high cortisol — linked to obesity — can also end up intensifying depression. The cycle gains momentum with each turn.
“Obesity and depression are bidirectional and multifactorial, so it’s really hard to unpick,” says Richard Morriss, a clinical psychiatrist and researcher at the University of Nottingham, UK. “The real kick in the teeth for someone who is both obese and depressed is that depression is fundamentally characterized by a loss in motivation, but to tackle obesity you need that motivation to eat better and exercise.”
Questions around treatment
What this might mean for treatment is just as challenging to understand. For starters, Morriss says awareness of the link between obesity and depression is low. He thinks obesity deserves to be treated with the same seriousness as anorexia. “Being too thin is seen as a mental-health problem,” he says. “But if you’re too overweight, it’s still primarily seen as a physical problem.”
When people with obesity who are depressed access treatment, the two conditions are often addressed separately, Morriss adds. “The psychological treatment for depression often ignores the obesity factor,” he says. Intervening to help one condition can inadvertently have negative consequences for the other; so the two should be closely monitored alongside each other.
Complicating matters, weight gain is a side effect of almost every antidepressant. “You take the medication to reduce depression, but it causes you to gain weight which worsens your depression, so you take more antidepressants, and so it goes on,” says Taylor.
Gaining weight isn’t the only concern for those with obesity taking antidepressants. In a 2021 study, Morriss and his colleagues investigated the medical records of more than 32,000 adults with obesity who also had depression. Those who were taking antidepressants had an increased risk of complications, including diabetes and cardiovascular problems5. It’s not entirely clear what is driving this trend, but it worries Morriss. “We concluded that people should be reviewed after being on antidepressants for 12 months,” he says. “We’re trying to discourage the idea that they should be on antidepressants permanently.” Other studies have shown a similar bump in the relative risk for these health concerns when it comes to antidepressant use in general populations6.
None of this is to say that antidepressants shouldn’t play an important part. In fact, Taylor recommends prioritizing depression over obesity. “You have to treat the depression first because you can’t make significant lifestyle changes until you’re mentally well,” she says. “You can’t do the work to lose weight while you’re actively depressed.” But physicians who want to take a holistic approach to the problem, she adds, need to consider the potentially adverse effects that antidepressants might have on people with obesity.
Tackling the obesity side of things isn’t straightforward either. In 2021, Himmerich and his colleagues conducted a systematic review of 24 studies that looked at obesity and depression7. This enabled the researchers to access data from more than 3,200 people with an aim of working out whether weight loss through dieting had the added bonus of also alleviating depression.
There’s been a lot of debate about what kind of diet is best to help lift people out of depression, says Himmerich. Key questions include whether it’s best to focus specifically on calorie reduction, and whether supplements such as omega-3 fatty acids and vitamins might be helpful. Himmerich concedes that there are no straightforward answers. “The science is not so clear because there are so many contradicting studies,” he says. “But our systematic review showed that calorie-restricted diets can decrease people’s depression score.”
There is an important caveat, however, for those who lose weight too rapidly. “People regain weight quickly after strict weight loss and can end up worse than they started,” says Himmerich. “So there needs to be a maintenance phase where people can be guided and instructed.”
Sadly, this kind of tailored therapy doesn’t exist for the vast majority of people with obesity and depression. “Patients can only find someone who can take them for part of the journey,” says Morriss. The combined problem of obesity and depression is unlikely to improve, he says, until therapeutic techniques evolve to confront and manage both problems.
"cycle" - Google News
August 24, 2022 at 08:50PM
https://ift.tt/eCmd6NV
The vicious cycle of depression and obesity - Nature.com
"cycle" - Google News
https://ift.tt/Fy1l0Xz
https://ift.tt/FHICvq9
Bagikan Berita Ini















0 Response to "The vicious cycle of depression and obesity - Nature.com"
Post a Comment